📋 At a Glance
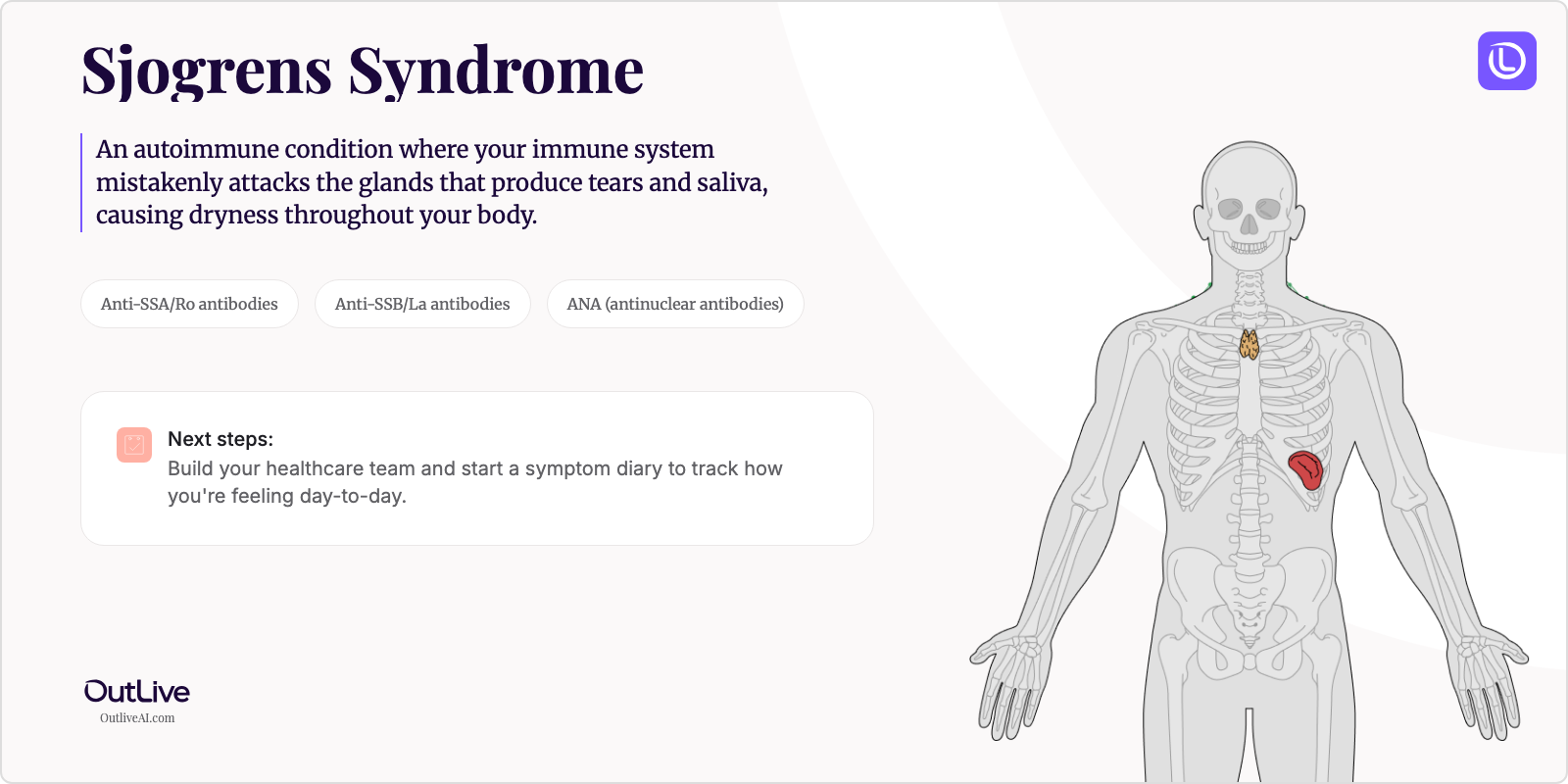
- What it is: An autoimmune condition where your immune system mistakenly attacks the glands that produce tears and saliva, causing dryness throughout your body.
- Key lab tests: Anti-SSA/Ro antibodies, Anti-SSB/La antibodies, and ANA (antinuclear antibodies)
- Your first goal: Build your healthcare team and start a symptom diary to track how you're feeling day-to-day.
Receiving a new diagnosis for Sjögren's Syndrome can be overwhelming. You might be feeling anxious, confused, and unsure of what comes next. That's completely normal. This guide is here to help you understand your condition in simple terms, know which lab tests matter most, and feel prepared for your next steps.
First, Take a Breath: What is Sjögren's Syndrome in Simple Terms?
Think of your body's moisture-producing glands like tiny sprinkler systems that keep your eyes, mouth, and other tissues comfortably moist. In Sjögren's Syndrome, your immune system—which normally protects you from germs—gets confused and starts attacking these "sprinkler systems." It's like having an overzealous security guard who mistakes the maintenance crew for intruders. This leads to the hallmark symptoms of dry eyes and dry mouth, though it can affect many other parts of your body too. The good news? While we can't cure it yet, we have many effective ways to manage your symptoms and help you feel better.
Understanding Your Diagnosis: The Key Lab Tests
This is the most important section. These are the main blood tests your doctor uses to diagnose and monitor Sjögren's Syndrome. Understanding what they mean will help you have more informed conversations with your healthcare team.
Key Tests for Sjögren's Syndrome:
- Anti-SSA/Ro Antibodies: These antibodies are found in about 40-60% of people with Sjögren's and help confirm your diagnosis when positive.
- Anti-SSB/La Antibodies: Almost always found alongside SSA antibodies, these are more specific to Sjögren's and rarely appear in other conditions.
- ANA (Antinuclear Antibodies): A general marker of autoimmune activity that's positive in about 50% of Sjögren's patients—think of it as a "check engine light" for autoimmune conditions.
- Rheumatoid Factor (RF): Often elevated in Sjögren's patients and can indicate more systemic involvement beyond just dryness symptoms.
Your First Specialist Appointment: What to Ask
What to Expect: You'll likely see a rheumatologist—a doctor who specializes in autoimmune conditions. They'll review your symptoms, examine you (checking for swollen glands and signs of dryness), and may order additional tests. The appointment typically lasts 30-45 minutes, and it's perfectly okay to bring a trusted person with you for support and to help remember information.
Questions to Ask Your Doctor:
- "How severe is my Sjögren's, and which organs are currently affected?"
- "What symptoms should I watch for that would require immediate attention?"
- "How often will I need follow-up appointments and blood work?"
- "Are there any medications that could be making my dryness worse that we should review?"
- "Should I see any other specialists, like an eye doctor or dentist who understands Sjögren's?"
Download our [Checklist of Questions to Ask Your Sjögren's Syndrome Specialist](# to feel prepared.
How to Track Your Journey
Tracking your Sjögren's Syndrome journey is crucial for understanding how your treatment is working and spotting important trends. Here's what you should monitor:
Symptoms to Track:
- Dry eyes and mouth severity (rate 1-10 daily)
- Fatigue levels and energy patterns throughout the day
- Joint pain or swelling locations and intensity
Lab Results to Monitor:
- Complete Blood Count (CBC) - Every 3-6 months to check for anemia or low white blood cells
- Inflammatory markers (ESR, CRP) - Every 3-6 months to track disease activity
- Kidney and liver function tests - Annually or as recommended, especially if on medications
Why Tracking Matters: Your symptoms can vary day to day, and it's easy to forget details between appointments. A tracking system helps you and your doctor see patterns—like whether fatigue worsens with weather changes or if a new treatment is actually helping. This information guides treatment adjustments and helps you feel more in control.
Next Steps After Your Diagnosis
Immediate Actions (This Week):
- Schedule appointments with an ophthalmologist familiar with Sjögren's for a baseline eye exam
- Visit your dentist to discuss your diagnosis and create a preventive care plan
- Start using preservative-free artificial tears and sugar-free lozenges for symptom relief
Short-term Goals (Next Month):
- Join a Sjögren's support group (online or in-person) to connect with others who understand
- Create a "moisture kit" for your home, work, and car with eye drops, lip balm, and water
- Begin a symptom diary to identify your personal triggers and patterns
Long-term Management:
- Establish regular check-ups with your rheumatologist every 3-6 months
- Develop a comprehensive dental care routine to prevent cavities and gum disease
Frequently Asked Questions
How quickly can I expect to feel better? Most people notice improvement in dryness symptoms within 2-4 weeks of starting treatment. Fatigue and joint pain may take 2-3 months to improve with medications like hydroxychloroquine. Remember, finding the right treatment combination is often a process—be patient with yourself.
Will I need to change my diet? While there's no specific "Sjögren's diet," many patients find that avoiding very dry, spicy, or acidic foods helps with mouth comfort. Staying well-hydrated and choosing moist foods can make eating more comfortable. Some people benefit from an anti-inflammatory diet rich in omega-3 fatty acids.
How often will I need to see my doctor? Initially, you'll likely see your rheumatologist every 3-4 months until your symptoms are stable. Once well-controlled, visits may stretch to every 6-12 months. You'll need regular dental cleanings every 3-4 months and eye exams every 6-12 months.
Can I still exercise/work/travel? Absolutely! Most people with Sjögren's maintain active lifestyles. Exercise actually helps with fatigue and joint pain. For travel, pack extra supplies of eye drops and medications, stay hydrated on flights, and consider a humidifier for hotel rooms.
When to Seek Immediate Medical Attention
Contact your doctor immediately if you experience:
- Sudden vision changes or severe eye pain that doesn't improve with drops
- Persistent fever, especially if on immunosuppressive medications
- Difficulty swallowing, severe mouth sores, or signs of oral infection
🔬 Ready to Organize Your Health Journey?
Understanding your condition is the first step. Our free Lab Analyzer tool helps you:
- Track all your lab results for Sjögren's Syndrome in one place
- Spot important trends over time
- Generate personalized questions for your doctor
[Upload Your Lab Report for Free Analysis →]