📋 At a Glance
- Inflammation markers like hs-CRP measure your body's inflammatory response, which can indicate infection, autoimmune disease, or heart disease risk
- hs-CRP specifically predicts cardiovascular risk, while other markers help diagnose and monitor various inflammatory conditions
- Fasting for 8-12 hours may provide more accurate results for heart disease risk assessment
If you're reading this, you've likely just had inflammation markers tested—especially hs-CRP—and are looking at results that might show "low risk," "moderate risk," or numbers that seem concerning. Take a breath. You're in the right place. This guide will walk you through what inflammation markers are, what your levels mean for your health, and most importantly, what you should do next. Think of us as your translator—we're here to help you understand your results so you can have a more informed conversation with your healthcare provider.
Why Are Inflammation Markers Ordered?
Your doctor might order inflammation markers for several reasons. Think of inflammation as your body's alarm system—it alerts you to problems like infections, injuries, or chronic diseases. But when this alarm stays on too long (chronic inflammation), it can damage your body and increase disease risk.
The most common reasons include:
Cardiovascular risk assessment: hs-CRP is a powerful predictor of heart attack and stroke risk, independent of cholesterol. It helps identify people who might benefit from more aggressive prevention.
Investigating unexplained symptoms: Fever, fatigue, weight loss, or general "not feeling well" might prompt testing to check for hidden inflammation.
Diagnosing inflammatory conditions: Elevated markers help diagnose conditions like rheumatoid arthritis, lupus, inflammatory bowel disease, or vasculitis.
Monitoring disease activity: In known inflammatory conditions, markers track whether treatment is working and if disease is active or in remission.
Infection detection: Very high levels often indicate bacterial infections, helping distinguish them from viral infections.
Post-surgery or injury monitoring: Markers track healing and can detect complications like infections or excessive inflammation.
Cancer screening support: Some cancers cause elevated inflammatory markers, though these tests alone can't diagnose cancer.
Evaluating chronic disease risk: Chronic low-grade inflammation is linked to diabetes, Alzheimer's, depression, and many other conditions.
Remember, inflammation isn't always bad—acute inflammation helps healing. It's chronic, low-grade inflammation that's particularly harmful over time.
How to Prepare for an Inflammation Markers Test
Proper preparation ensures the most accurate results:
Fasting considerations:
- For hs-CRP heart risk assessment: 8-12 hour fast recommended
- For general inflammation testing: Usually no fasting required
- Follow your doctor's specific instructions
Timing is important:
- Don't test during acute illness (cold, flu, infection)
- Wait 2-3 weeks after illness or injury for baseline testing
- Avoid testing right after dental work or procedures
- For women: Inflammation can vary with menstrual cycle
Activity and lifestyle:
- Avoid strenuous exercise 24 hours before testing
- Don't drink alcohol 24 hours before
- Continue regular medications unless instructed otherwise
- Note any recent stress or poor sleep
Medications to mention:
- NSAIDs (ibuprofen, naproxen)
- Steroids (prednisone)
- Statins (can lower CRP)
- Hormone replacement therapy
- Birth control pills
Supplements that may affect results:
- Omega-3 fatty acids
- Turmeric/curcumin
- Vitamin D
- Probiotics
The blood draw is routine—typically one or two tubes. Results usually come back within 1-3 days.
Understanding the Components of Your Inflammation Markers Report
Your inflammation markers tell different stories about what's happening in your body. Each test provides unique information about the type, severity, and possible cause of inflammation.
What Do the Main Inflammation Tests Mean?
These are the most commonly ordered inflammation markers:
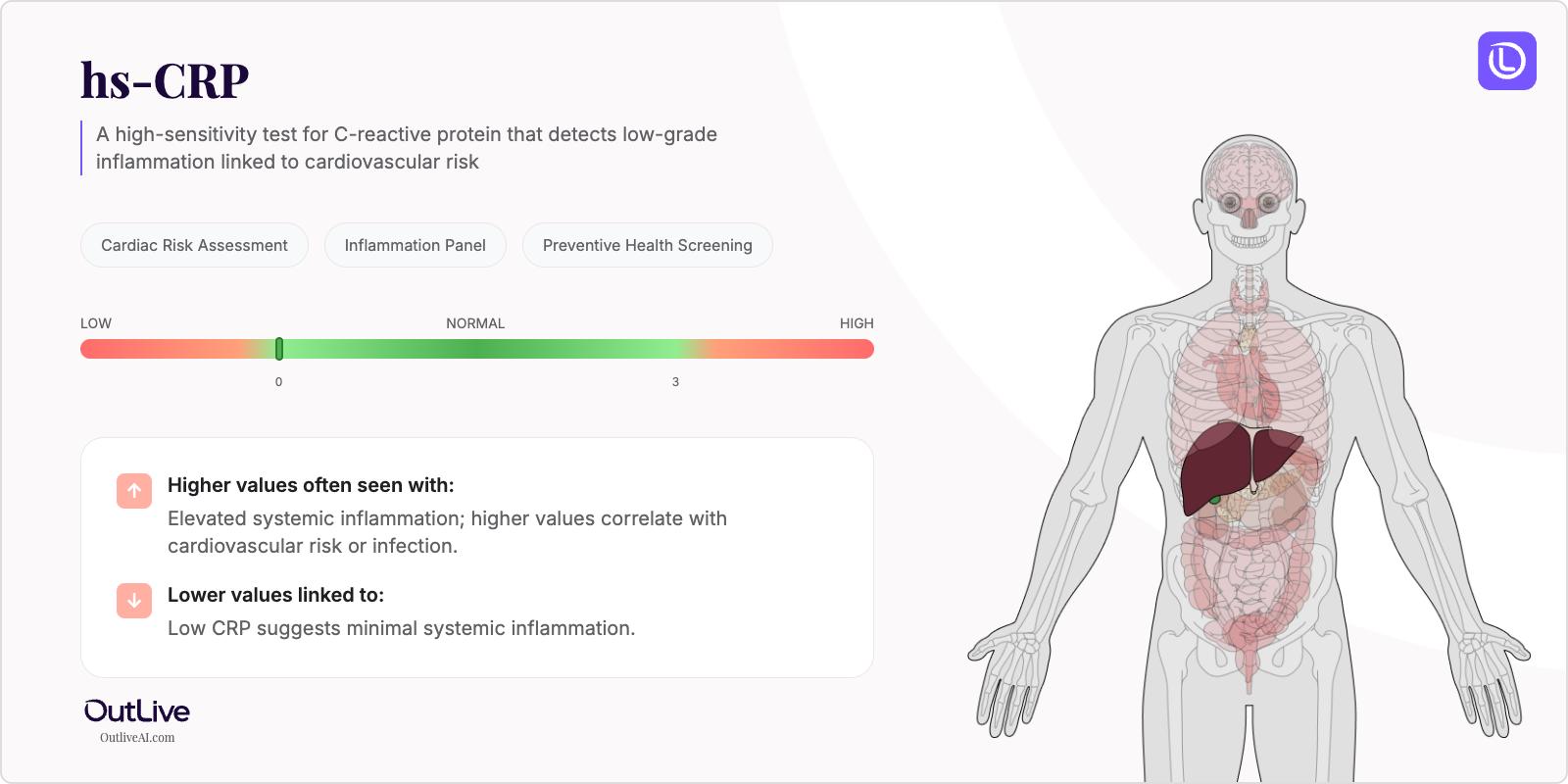
hs-CRP (High-Sensitivity C-Reactive Protein): The gold standard for measuring low-grade inflammation and cardiovascular risk. Think of it as your body's smoke detector—it rises quickly with any inflammation. The "high-sensitivity" version detects even small amounts that predict heart disease risk.
CRP (Standard C-Reactive Protein): Measures higher levels of inflammation from infections or inflammatory diseases. Same protein as hs-CRP but less sensitive test. Used for detecting active infections or monitoring inflammatory conditions.
ESR (Erythrocyte Sedimentation Rate): Measures how quickly red blood cells settle in a tube. Inflammation makes them clump and fall faster. It's like watching sediment settle in water—faster settling means more inflammation. ESR rises slowly and falls slowly, showing inflammation over weeks.
Ferritin: While primarily an iron storage marker, ferritin rises significantly with inflammation, which can mask iron deficiency. Very high levels might indicate Still's disease or hemophagocytic syndrome.
Fibrinogen: A clotting protein that rises with inflammation. Elevated levels increase both inflammation and clot risk, making it a double cardiovascular threat.
Here are the typical ranges for main inflammation markers:
| Test | Low/Normal | Moderate | High | Very High |
|---|---|---|---|---|
| hs-CRP (cardiac risk) | \ <1.0mg/L | 1.0-3.0 mg/L | 3.0-10.0 mg/L | \ >10.0mg/L* |
| CRP (inflammation) | \ <3.0mg/L | 3.0-10.0 mg/L | 10.0-100 mg/L | \ >100mg/L |
| ESR (male) | 0-15 mm/hr | 15-30 mm/hr | 30-60 mm/hr | \ >60mm/hr |
| ESR (female) | 0-20 mm/hr | 20-35 mm/hr | 35-70 mm/hr | \ >70mm/hr |
| Ferritin (inflammatory) | Normal range | 2-3x normal | 3-5x normal | \ >5x normal |
| Fibrinogen | 200-400 mg/dL | 400-500 mg/dL | 500-700 mg/dL | \ >700mg/dL |
*hs-CRP >10 mg/L suggests acute inflammation, not just cardiac risk
What Do Specialized Inflammation Tests Mean?
Additional markers for specific conditions:
Procalcitonin: Specifically rises with bacterial infections, especially sepsis. Helps distinguish bacterial from viral infections. Critical for antibiotic decisions in hospitals.
IL-6 (Interleukin-6): A cytokine that triggers CRP production. Rises earlier than CRP in inflammation. Particularly important in cytokine storm syndromes and some cancers.
TNF-alpha (Tumor Necrosis Factor): Key inflammatory cytokine in autoimmune diseases. Target of biologic drugs like Humira and Remicade. Elevated in rheumatoid arthritis, Crohn's disease.
Calprotectin (stool): Specifically indicates intestinal inflammation. Distinguishes inflammatory bowel disease from irritable bowel syndrome. Monitors IBD activity.
Anti-CCP Antibodies: Specific for rheumatoid arthritis. Often positive before symptoms appear. Predicts more aggressive disease.
ANA (Antinuclear Antibodies): Screens for autoimmune diseases like lupus. Pattern and titer provide additional information.
What Do Abnormal Results Mean? (A High-Level Guide)
Inflammation marker interpretation depends on the clinical context, pattern of elevation, and other symptoms:
Cardiovascular Risk Pattern (hs-CRP):
- <1.0 mg/L: Low risk
- 1.0-3.0 mg/L: Moderate risk (consider lifestyle changes)
- >3.0 mg/L: High risk (aggressive risk reduction needed)
- Persistent elevation over multiple tests most significant
- Combined with cholesterol for better risk prediction
Acute Infection Pattern:
- CRP: 10-100+ mg/L (bacterial usually higher than viral)
- ESR: Moderately elevated
- Procalcitonin: Elevated in bacterial infections
- Ferritin: May be elevated
- Usually with fever, elevated white blood cells
Autoimmune Disease Pattern:
- CRP and ESR: Persistently elevated
- Specific antibodies positive (Anti-CCP, ANA, etc.)
- Ferritin may be high
- Correlates with disease activity
- Examples: Rheumatoid arthritis, lupus, vasculitis
Inflammatory Bowel Disease Pattern:
- CRP and ESR elevated during flares
- Calprotectin (stool) elevated
- Helps distinguish from IBS
- Monitors treatment response
- Examples: Crohn's disease, ulcerative colitis
Chronic Low-Grade Inflammation:
- hs-CRP: 3-10 mg/L persistently
- Associated conditions:
- Obesity (fat tissue produces inflammatory markers)
- Type 2 diabetes
- Metabolic syndrome
- Depression
- Chronic stress
- Poor sleep
- Sedentary lifestyle
Cancer-Associated Pattern:
- Variable elevation of CRP and ESR
- Very high ferritin in some cancers
- Not specific—many cancers don't elevate markers
- Used for monitoring, not diagnosis
Post-Surgical/Trauma Pattern:
- CRP peaks at 48-72 hours post-surgery
- Gradual decline expected
- Persistent elevation suggests complications
- ESR stays elevated longer than CRP
Important Special Considerations:
Factors that raise inflammatory markers:
- Obesity (especially abdominal)
- Smoking
- Chronic stress
- Poor sleep
- Western diet (high sugar, processed foods)
- Sedentary lifestyle
- Chronic infections
- Air pollution
Factors that lower inflammatory markers:
- Regular exercise
- Mediterranean diet
- Weight loss
- Omega-3 fatty acids
- Good sleep
- Stress management
- Certain medications (statins, aspirin)
Important disclaimer: Inflammatory markers are non-specific—they indicate inflammation exists but not always the cause. High levels require investigation but don't diagnose specific conditions. Very high levels need urgent evaluation. Only your healthcare provider can interpret results in context with symptoms and other tests. Never ignore persistently elevated markers.
Next Steps After Your Inflammation Markers Test
So you've read through your results—what now? Here's your action plan:
1. Schedule a follow-up with your doctor: Elevated markers always need investigation to find the cause and determine if treatment is needed.
2. Prepare your questions: Not sure what to ask? We've created a helpful checklist of questions to bring to your appointment. [Download our Inflammation Markers Doctor Questions Checklist](# to make sure you cover everything important.
3. Based on your results:
If hs-CRP shows cardiac risk (1-10 mg/L):
- Repeat test to confirm (single test can be misleading)
- Comprehensive cardiovascular assessment
- Consider advanced lipid testing
- Aggressive lifestyle modification
- Possible statin therapy even with normal cholesterol
If markers suggest infection/acute inflammation:
- Identify and treat source
- May need antibiotics or other treatment
- Recheck after treatment
- Ensure complete resolution
If pattern suggests autoimmune disease:
- Referral to rheumatologist
- Additional specific antibody tests
- Imaging studies
- Early treatment prevents damage
4. Reduce inflammation naturally:
- Diet: Mediterranean diet, omega-3s, reduce sugar/processed foods
- Exercise: Regular moderate activity (150 min/week)
- Weight: Even 5-10% loss significantly reduces inflammation
- Sleep: 7-9 hours nightly
- Stress: Meditation, yoga, therapy
- Stop smoking: Major inflammation trigger
5. Monitor your levels:
- Retest based on condition and treatment
- Track trends over time
- Adjust treatment based on response
- Some conditions need lifelong monitoring
6. Know when to seek immediate care:
- Very high CRP (>100 mg/L)
- Fever with elevated markers
- Chest pain with elevated hs-CRP
- Severe joint pain/swelling
🔬 Ready to Translate Your Full Report?
Understanding your inflammation markers is just the beginning. Our free Lab Analyzer tool helps you:
- Track all your lab results in one place
- Spot important trends over time
- Generate personalized questions for your doctor
- Get plain-English explanations of every test
[Upload Your Lab Report for Free Analysis →]
Join 50,000+ people taking control of their health journey
Remember, knowledge is power when it comes to your health. Understanding your inflammation markers helps you and your healthcare provider identify hidden health risks and monitor treatment effectiveness. While inflammation is a complex process, managing it through lifestyle changes and appropriate treatment can significantly improve your health outcomes. You've already taken the first step by educating yourself—now work with your healthcare provider to address any inflammation and protect your long-term health.