📋 At a Glance
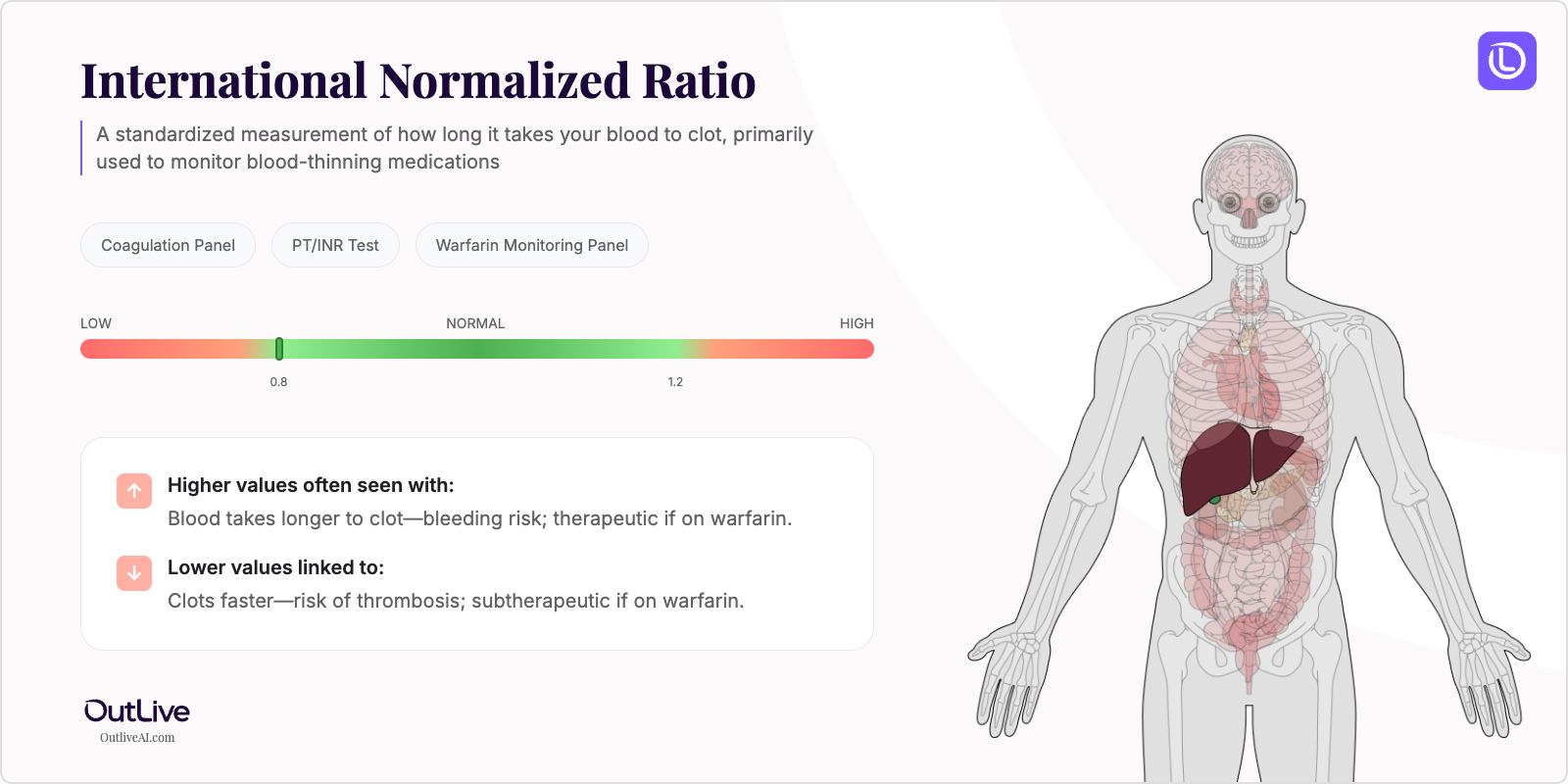
- What it is: A standardized measurement of how long it takes your blood to clot, primarily used to monitor blood-thinning medications
- Found in tests: Coagulation Panel, PT/INR Test, Warfarin Monitoring Panel
- Normal range: 0.8-1.2 for people not on blood thinners; 2.0-3.0 for most people on warfarin
If you're looking at your lab results and wondering what INR means, you're in the right place. Think of INR as your blood's "clotting speed score" - it tells us how quickly or slowly your blood forms clots compared to normal. Just like a traffic light controls the flow of cars, your INR helps doctors understand if your blood is flowing too freely (high INR) or clotting too quickly (low INR). Let's break down what your numbers mean in plain English.
Why Is INR Tested?
Your doctor orders an INR test primarily to monitor how well blood-thinning medications like warfarin (Coumadin) are working. It's like checking the thermostat to make sure your home's temperature is just right - not too hot, not too cold. The INR helps ensure your medication dose keeps your blood in that "Goldilocks zone" where it won't clot unnecessarily but can still stop bleeding when needed.
This test is also ordered before surgeries to ensure your blood can clot properly during and after the procedure. Sometimes, doctors use it to investigate unexplained bleeding or bruising, check liver function (since your liver makes clotting proteins), or evaluate clotting disorders. If you have conditions like atrial fibrillation, deep vein thrombosis, or artificial heart valves, regular INR monitoring becomes part of your routine care.
The INR is particularly important because it standardizes results across different laboratories worldwide. Before INR existed, different labs could report different numbers for the same blood sample, making it difficult to manage medications consistently. Now, whether you're tested in New York or Tokyo, your INR means the same thing.
What Does INR Do in Your Body?
The INR doesn't actually "do" anything in your body - it's a calculated measurement that reflects how your blood's clotting system is working. Your blood contains special proteins called clotting factors, made primarily by your liver using vitamin K. These factors work together like a perfectly choreographed dance team to form clots when you're injured.
When you take blood-thinning medications, they interfere with vitamin K's ability to help produce these clotting factors. This slows down the clotting process, which is exactly what we want for certain medical conditions. The INR measures this slowdown by comparing your clotting time to a standard reference. An INR of 2.0 means your blood takes twice as long to clot as normal blood, while an INR of 3.0 means it takes three times as long.
Your INR is closely related to other clotting tests, particularly the Prothrombin Time (PT). In fact, INR is calculated from your PT result using a special formula that accounts for variations in testing methods. This relationship helps doctors get a complete picture of your clotting system's health and ensures your treatment is properly adjusted.
What Do My INR Results Mean?
Normal INR Ranges
| Population | Normal Range | Therapeutic Range (on warfarin) |
|---|---|---|
| Adult Male (not on anticoagulants) | 0.8-1.2 | 2.0-3.0 (standard therapy) |
| Adult Female (not on anticoagulants) | 0.8-1.2 | 2.0-3.0 (standard therapy) |
| Children (not on anticoagulants) | 0.8-1.2 | 2.0-3.0 (when indicated) |
| Mechanical heart valve patients | 0.8-1.2 (baseline) | 2.5-3.5 (higher target) |
| Pregnancy | 0.8-1.2 | Varies by trimester and indication |
Note: Reference ranges may vary slightly between laboratories. Always compare your results to the range provided on your specific lab report.
What Does High INR Mean?
Common Causes:
- Warfarin dose too high: The most common cause in patients on blood thinners
- Vitamin K deficiency: From poor diet, malabsorption, or prolonged antibiotic use
- Liver disease: Cirrhosis, hepatitis, or liver failure affecting clotting factor production
- Drug interactions: Antibiotics, antifungals, or NSAIDs interfering with warfarin
- Dietary changes: Sudden decrease in vitamin K-rich foods (leafy greens)
- Alcohol consumption: Binge drinking or chronic alcohol use affecting liver function
- Inherited clotting disorders: Rare genetic conditions affecting clotting factors
Possible Symptoms:
- Easy bruising or bruises appearing without injury
- Bleeding gums when brushing teeth
- Nosebleeds that are hard to stop
- Blood in urine (pink or red colored)
- Dark, tarry stools or bright red blood in stool
- Unusually heavy menstrual periods
- Prolonged bleeding from cuts
When to Be Concerned: An INR above 4.0 significantly increases bleeding risk and requires immediate medical attention. If your INR is above 5.0, or if you experience signs of serious bleeding (severe headache, vomiting blood, confusion, weakness on one side of the body), seek emergency care immediately. Even without symptoms, an INR above your target range needs prompt adjustment of your medication.
What Does Low INR Mean?
Common Causes:
- Warfarin dose too low: Insufficient medication to prevent clotting
- Missed doses: Forgetting to take warfarin as prescribed
- Vitamin K excess: Eating large amounts of leafy greens or taking supplements
- Drug interactions: Medications that reduce warfarin's effectiveness
- Genetic variations: Some people metabolize warfarin differently
- Malabsorption issues: Conditions affecting how you absorb medications
- Thyroid disorders: Hyperthyroidism can lower INR levels
Possible Symptoms:
- Leg pain, swelling, or warmth (possible blood clot)
- Chest pain or shortness of breath
- Sudden vision changes
- Numbness or weakness in face, arm, or leg
- Severe headache
- Difficulty speaking or understanding speech
When to Be Concerned: If you're on warfarin and your INR falls below 2.0, you're at increased risk for dangerous blood clots. Seek immediate medical attention if you experience symptoms of a blood clot or stroke. Your doctor will likely adjust your medication dose and may order additional tests to ensure you're protected.
What Can Affect My INR Levels?
Factors That May Increase Levels:
- Medications: Antibiotics (especially metronidazole, sulfamethoxazole), antifungals (fluconazole), amiodarone, aspirin, NSAIDs
- Lifestyle: Alcohol consumption, sudden dietary changes, illness or fever, diarrhea
- Conditions: Liver disease, hyperthyroidism, heart failure, recent surgery
- Supplements: Vitamin E, garlic, ginkgo biloba, ginger, fish oil, cranberry products
Factors That May Decrease Levels:
- Medications: Rifampin, carbamazepine, oral contraceptives, vitamin K supplements
- Lifestyle: High intake of vitamin K foods (kale, spinach, broccoli), consistent exercise routine
- Conditions: Hypothyroidism, increased vitamin K absorption, genetic factors
- Time of Day: Minor variations can occur, though less significant than other factors
How Is INR Related to Other Tests?
Your INR is calculated from your Prothrombin Time (PT) test, making them inseparable partners in monitoring your clotting system. It's often ordered alongside a Complete Blood Count (CBC) to check platelet levels and ensure all components of clotting are working properly.
Often tested alongside: PT (Prothrombin Time), aPTT (activated Partial Thromboplastin Time), Platelet Count, Liver Function Tests Part of: Coagulation Panel, Pre-surgical Testing Panel Ratio calculations: INR = (Patient PT / Control PT)^ISI Follow-up tests: If abnormal, your doctor might order Factor assays, Liver function tests, or Vitamin K levels
Frequently Asked Questions
How often should INR be tested? When starting warfarin, you'll need testing every few days until stable, then weekly, then monthly once your dose is established. Most stable patients test monthly, but any medication changes or illness may require more frequent monitoring.
Can I improve my INR levels naturally? If you're on warfarin, never try to adjust your INR through diet alone - work with your doctor. However, maintaining consistent vitamin K intake (rather than avoiding it completely) helps keep your INR stable.
Should I fast before an INR test? No fasting is required for an INR test. You can eat and drink normally before your blood draw.
How quickly can INR levels change? INR can change within 24-48 hours after a warfarin dose adjustment. Diet changes or new medications can affect INR within 2-3 days. This is why consistency in diet and medication timing is so important.
Next Steps After Your INR Test
Questions to Ask Your Doctor:
- What do my INR results mean for my overall health?
- Are my levels related to my symptoms?
- Do I need additional testing?
- Should we monitor this over time?
- Are there lifestyle changes that could help?
- How do my other medications affect my INR?
- What foods should I eat consistently rather than avoid?
Download our INR Doctor Questions Checklist
🔬 Ready to Track Your INR Over Time?
Understanding a single INR result is just the beginning. Our free Lab Analyzer tool helps you:
- Track how your INR changes over time
- See how it relates to your other lab values
- Identify patterns your doctor might miss
- Get personalized insights based on your trends
[Upload Your Lab Report for Free Analysis →]