📋 At a Glance
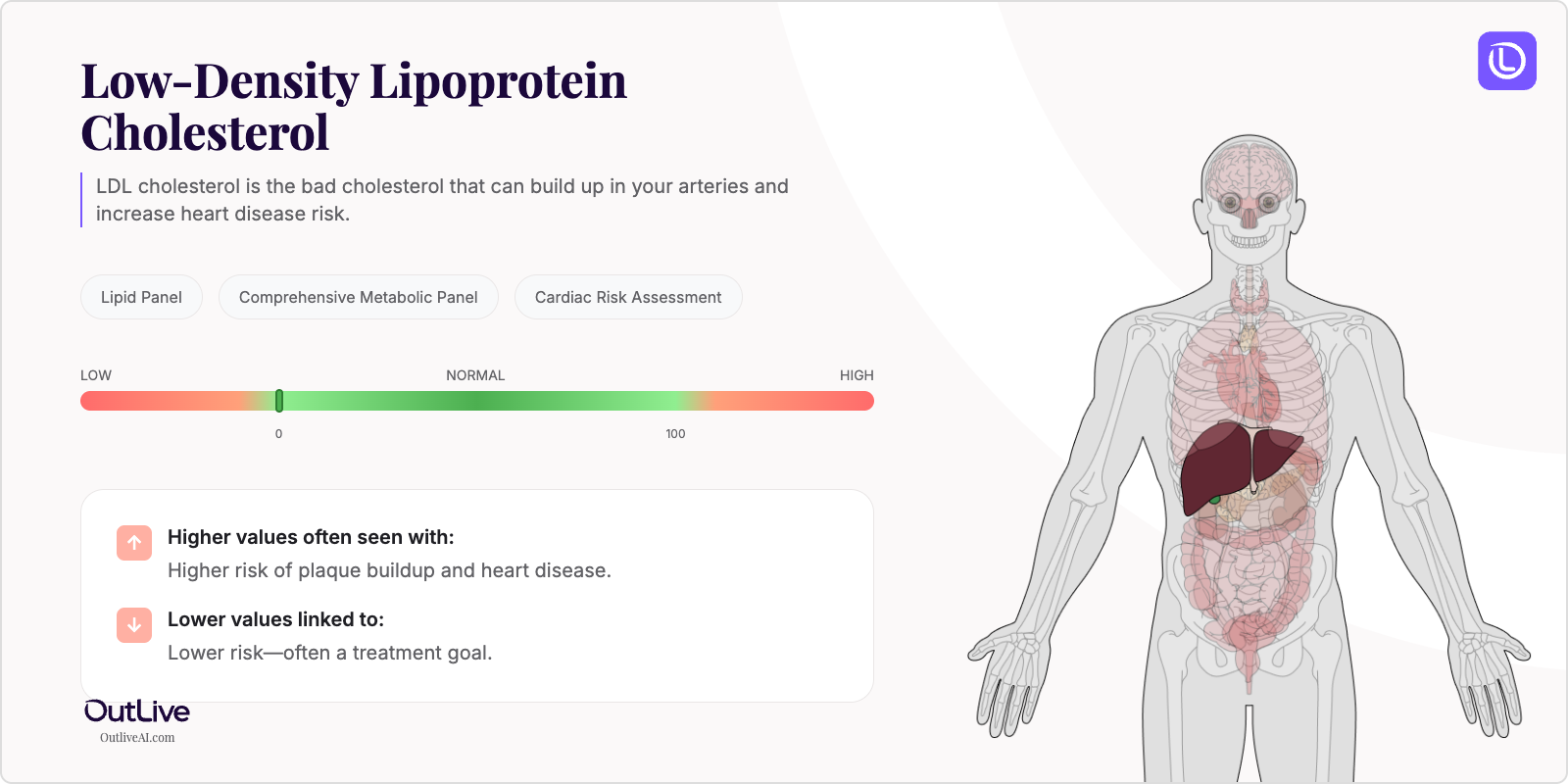
- What it is: LDL cholesterol is the "bad" cholesterol that can build up in your arteries and increase heart disease risk.
- Found in tests: Lipid Panel, Comprehensive Metabolic Panel, Cardiac Risk Assessment
- Normal range: Less than 100 mg/dL is optimal for most adults
If you're looking at your lab results and wondering what LDL cholesterol means, you're in the right place. Think of LDL as delivery trucks carrying cholesterol through your bloodstream – while you need some deliveries, too many trucks can cause a traffic jam in your arteries. Let's break down what your numbers mean in plain English, so you can have a more informed conversation with your doctor.
Why Is LDL Cholesterol Tested?
Your doctor orders an LDL cholesterol test as part of routine health screening, typically starting at age 20 and repeating every 4-6 years if your levels are normal. It's a crucial component of your lipid panel, which gives us a complete picture of your heart health risk. If you have diabetes, high blood pressure, or a family history of heart disease, your doctor may check it more frequently – perhaps annually or even every few months while adjusting medications.
This test becomes especially important if you're experiencing symptoms that might suggest cardiovascular issues, such as chest pain, shortness of breath, or if you've had a stroke or heart attack. We also monitor LDL closely when you're taking cholesterol-lowering medications to ensure they're working effectively. Remember, high LDL rarely causes symptoms until significant damage has occurred, which is why regular screening is so valuable – it's like checking your car's oil before the engine light comes on.
What Does LDL Cholesterol Do in Your Body?
LDL stands for Low-Density Lipoprotein, and despite its "bad" reputation, your body actually needs some LDL to function properly. These particles carry cholesterol from your liver to cells throughout your body, where it's used to build cell membranes, produce hormones like estrogen and testosterone, and create vitamin D. Think of LDL particles as essential delivery vehicles – the problem arises when there are too many deliveries and not enough customers.
When LDL levels are too high, these cholesterol-carrying particles can get stuck in your artery walls, especially if the arteries have been damaged by high blood pressure, smoking, or inflammation. Over time, this creates plaques that narrow your arteries, much like how mineral deposits can clog your home's pipes. Your liver produces most of your LDL cholesterol, but diet also plays a significant role, particularly foods high in saturated and trans fats.
What Do My LDL Results Mean?
Normal LDL Ranges
| Population | Normal Range | Optimal Range |
|---|---|---|
| Adult Male | Less than 130 mg/dL | Less than 100 mg/dL |
| Adult Female | Less than 130 mg/dL | Less than 100 mg/dL |
| Children (2-19 years) | Less than 110 mg/dL | Less than 90 mg/dL |
| Pregnancy | May increase 25-50% | Consult your OB/GYN |
| High-risk patients* | Less than 100 mg/dL | Less than 70 mg/dL |
*High-risk includes those with diabetes, heart disease, or multiple risk factors Note: Reference ranges may vary slightly between laboratories. Always compare your results to the range provided on your specific lab report.
What Does High LDL Mean?
Common Causes:
- Diet high in saturated fats: Red meat, full-fat dairy, fried foods, and processed snacks can significantly raise LDL
- Genetic conditions: Familial hypercholesterolemia affects 1 in 250 people and causes very high LDL from birth
- Hypothyroidism: An underactive thyroid slows your body's ability to clear LDL from the blood
- Diabetes: High blood sugar damages blood vessels and often leads to increased LDL production
- Kidney disease: Impaired kidney function affects how your body processes cholesterol
- Medications: Certain drugs like steroids, some blood pressure medications, and HIV treatments can raise LDL
- Sedentary lifestyle: Lack of physical activity reduces your body's ability to process cholesterol effectively
Possible Symptoms:
- Usually no symptoms until complications develop
- Yellowish deposits around eyes (xanthelasma)
- Fatty deposits on tendons (xanthomas)
- Chest pain or pressure (if arteries are significantly blocked)
When to Be Concerned: LDL levels above 160 mg/dL are considered high, and levels above 190 mg/dL are very high, requiring immediate attention. If your LDL is above 190 mg/dL, or above 160 mg/dL with other risk factors like diabetes or smoking, your doctor will likely recommend medication along with lifestyle changes. Don't panic – high LDL is treatable, but it does require action to prevent heart disease and stroke.
What Does Low LDL Mean?
Common Causes:
- Cholesterol-lowering medications: Statins and other drugs working effectively
- Hyperthyroidism: An overactive thyroid speeds up cholesterol metabolism
- Malnutrition or malabsorption: Conditions affecting nutrient absorption like celiac disease
- Liver disease: Advanced liver disease impairs cholesterol production
- Certain cancers: Some blood cancers can cause very low cholesterol
- Genetic conditions: Rare disorders like abetalipoproteinemia
- Extreme diets: Very low-fat diets or eating disorders
Possible Symptoms:
- Usually no symptoms from low LDL itself
- Fatigue or weakness (if related to underlying condition)
- Depression or mood changes (cholesterol is needed for brain function)
- Poor wound healing
When to Be Concerned: While we often focus on high LDL, levels below 40 mg/dL may warrant investigation, especially if they drop suddenly or are accompanied by other abnormal lab results. Very low LDL isn't necessarily harmful by itself, but it might signal an underlying condition that needs attention.
What Can Affect My LDL Levels?
Factors That May Increase Levels:
- Medications: Birth control pills, thiazide diuretics, beta-blockers, anabolic steroids
- Lifestyle: Weight gain, smoking, excessive alcohol, stress, lack of sleep
- Conditions: Pregnancy, menopause, winter months (less vitamin D), recent illness
- Supplements: Some protein powders, excessive vitamin A
Factors That May Decrease Levels:
- Medications: Statins, PCSK9 inhibitors, bile acid sequestrants, fibrates
- Lifestyle: Regular exercise, Mediterranean diet, weight loss, quitting smoking
- Conditions: Acute illness, recent surgery, hyperthyroidism
- Time of Day: LDL can be slightly lower in the afternoon
How Is LDL Cholesterol Related to Other Tests?
Your LDL cholesterol is part of a bigger picture that includes several related measurements. It's always tested alongside HDL (the "good" cholesterol), total cholesterol, and triglycerides as part of your lipid panel. Your doctor may calculate ratios like total cholesterol/HDL or look at non-HDL cholesterol (total minus HDL) for a more complete risk assessment.
Often tested alongside: HDL cholesterol, triglycerides, total cholesterol, apolipoprotein B Part of: Lipid Panel, Cardiac Risk Panel Ratio calculations: Total cholesterol/HDL ratio, LDL/HDL ratio Follow-up tests: If LDL is high, your doctor might order thyroid function tests, liver enzymes, or inflammatory markers like CRP
Frequently Asked Questions
How often should LDL be tested? For adults with normal levels and no risk factors, every 4-6 years is sufficient. If you have high LDL, diabetes, or heart disease, your doctor may check it every 3-12 months, especially when starting or adjusting medications.
Can I improve my LDL levels naturally? Absolutely! Many people can lower LDL by 20-30% through lifestyle changes alone: adopting a Mediterranean-style diet, exercising 150 minutes weekly, losing 5-10% of body weight if overweight, and adding soluble fiber and plant sterols to your diet.
Should I fast before an LDL test? Traditionally, a 9-12 hour fast was required, but recent guidelines suggest non-fasting tests are acceptable for most people. However, your doctor may still request fasting for the most accurate results, especially if your triglycerides are high.
How quickly can LDL levels change? Diet changes can affect LDL within 2-3 weeks, while statins typically show results in 4-6 weeks. Maximum lifestyle benefits usually appear after 3-6 months of consistent healthy habits.
Next Steps After Your LDL Test
Questions to Ask Your Doctor:
- What do my LDL results mean for my overall heart disease risk?
- Are my levels related to my family history or lifestyle?
- Do I need additional testing like an apolipoprotein B or calcium score?
- Should we monitor this over time, and how often?
- Are there specific dietary changes that would help my situation?
- Would medication be beneficial, and what are the pros and cons?
Download our LDL Cholesterol Doctor Questions Checklist
🔬 Ready to Track Your LDL Cholesterol Over Time?
Understanding a single LDL result is just the beginning. Our free Lab Analyzer tool helps you:
- Track how your LDL changes over time
- See how it relates to your other lab values
- Identify patterns your doctor might miss
- Get personalized insights based on your trends
[Upload Your Lab Report for Free Analysis →]