📋 At a Glance
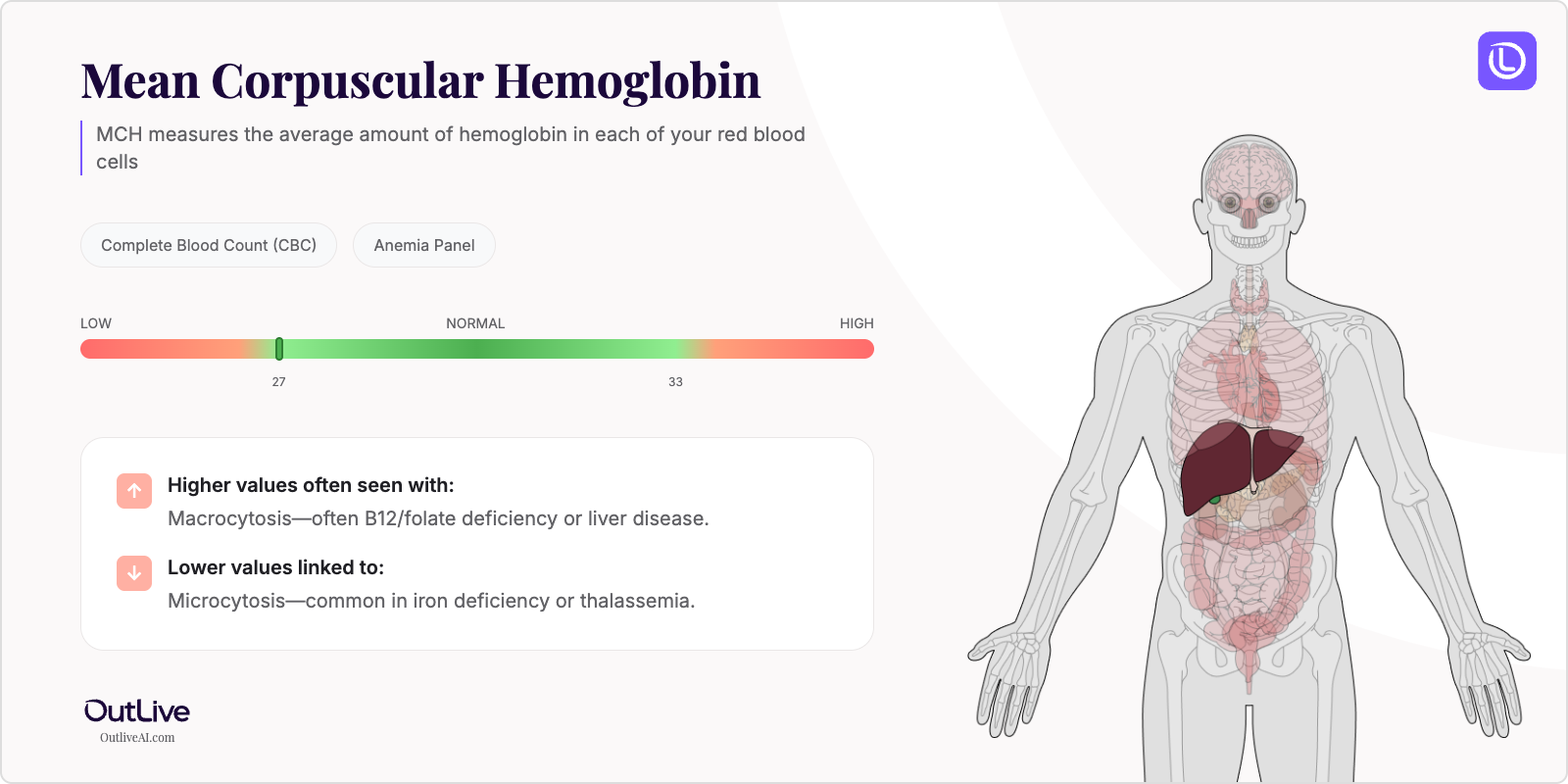
- What it is: MCH measures the average amount of hemoglobin in each of your red blood cells
- Found in tests: Complete Blood Count (CBC), Anemia Panel
- Normal range: 27-33 picograms per cell (pg/cell)
If you're looking at your lab results and wondering what MCH means, you're in the right place. Think of MCH as a quality control measure for your red blood cells – like checking if each delivery truck in your body's fleet is carrying the right amount of oxygen packages. Let's break down what your numbers mean in plain English, so you can walk into your next doctor's appointment feeling informed and confident.
Why Is MCH Tested?
Your doctor orders an MCH test as part of a Complete Blood Count (CBC), one of the most common blood tests in medicine. It's like a health report card for your blood, and MCH is one of the important grades on that card. This test is routinely included in annual check-ups, pre-surgery evaluations, and when you're experiencing symptoms like fatigue, weakness, or shortness of breath.
MCH becomes particularly important when your doctor suspects anemia or other blood disorders. If you've been feeling unusually tired, looking pale, or experiencing dizziness, your MCH level helps paint a picture of what's happening inside your red blood cells. It's especially valuable because it can help distinguish between different types of anemia – think of it as helping your doctor identify not just that there's a problem, but what specific type of problem you're dealing with.
The test also monitors how well you're responding to treatments for blood conditions. If you're taking iron supplements or receiving vitamin B12 injections, your MCH levels help track whether the treatment is working. It's like having a progress meter that shows if your body is successfully rebuilding its oxygen-carrying capacity.
What Does MCH Do in Your Body?
MCH stands for Mean Corpuscular Hemoglobin, which sounds complicated but is actually quite simple. "Mean" just means average, "corpuscular" refers to your red blood cells, and "hemoglobin" is the protein that carries oxygen. So MCH tells us the average amount of hemoglobin packed into each of your red blood cells.
Imagine your red blood cells as tiny taxis, and hemoglobin as the passengers they carry. MCH measures how many passengers are in each taxi on average. Too few passengers (low MCH) means each taxi isn't carrying enough oxygen to your tissues. Too many passengers (high MCH) might mean the taxis are overloaded or unusually large, which can also cause problems.
Your bone marrow produces these red blood cells, and they need the right building blocks – iron, vitamin B12, and folate – to load them with the proper amount of hemoglobin. When everything's working correctly, each red blood cell carries just the right amount of hemoglobin to efficiently deliver oxygen from your lungs to every corner of your body. This balance is crucial because your brain, heart, muscles, and every other organ depend on this steady oxygen supply to function properly.
What Do My MCH Results Mean?
Normal MCH Ranges
| Population | Normal Range | Optimal Range |
|---|---|---|
| Adult Male | 27-33 pg/cell | 29-31 pg/cell |
| Adult Female | 27-33 pg/cell | 29-31 pg/cell |
| Children (6-12 years) | 25-33 pg/cell | 27-31 pg/cell |
| Pregnancy | 27-32 pg/cell | 28-31 pg/cell |
Note: Reference ranges may vary slightly between laboratories. Always compare your results to the range provided on your specific lab report.
What Does High MCH Mean?
Common Causes:
- Vitamin B12 deficiency - Your body can't properly form red blood cells without enough B12, leading to larger cells with more hemoglobin
- Folate deficiency - Similar to B12, low folate causes your bone marrow to produce abnormally large red blood cells
- Macrocytic anemia - A condition where red blood cells are larger than normal and contain excess hemoglobin
- Liver disease - Your liver plays a role in processing nutrients needed for healthy red blood cells
- Hypothyroidism - An underactive thyroid can affect red blood cell production
- Certain medications - Some HIV medications, chemotherapy drugs, and anti-seizure medications can elevate MCH
- Alcohol use disorder - Chronic alcohol consumption interferes with vitamin absorption and red blood cell formation
Possible Symptoms:
- Fatigue and weakness
- Shortness of breath
- Pale or yellowish skin
- Tingling or numbness in hands and feet
- Difficulty with balance or coordination
- Memory problems or confusion
When to Be Concerned: If your MCH is above 35 pg/cell and you're experiencing neurological symptoms like numbness, tingling, or balance problems, contact your healthcare provider promptly. These could indicate a severe B12 deficiency that needs immediate treatment to prevent permanent nerve damage.
What Does Low MCH Mean?
Common Causes:
- Iron deficiency anemia - The most common cause; without enough iron, your body can't make adequate hemoglobin
- Thalassemia - An inherited blood disorder affecting hemoglobin production
- Chronic blood loss - From heavy periods, ulcers, or other sources of bleeding
- Chronic kidney disease - Your kidneys produce a hormone that stimulates red blood cell production
- Lead poisoning - Lead interferes with hemoglobin synthesis
- Inflammatory conditions - Chronic inflammation can affect iron metabolism
- Celiac disease - Can cause poor iron absorption in the intestines
Possible Symptoms:
- Extreme fatigue and weakness
- Rapid heartbeat or palpitations
- Headaches and dizziness
- Cold hands and feet
- Brittle nails or spoon-shaped nails
- Frequent infections
- Unusual cravings for ice, dirt, or starch
When to Be Concerned: If your MCH is below 25 pg/cell and you're experiencing chest pain, severe shortness of breath, or rapid heartbeat, seek medical attention immediately. These symptoms could indicate your body isn't getting enough oxygen and needs urgent evaluation.
What Can Affect My MCH Levels?
Factors That May Increase Levels:
- Medications: Metformin (diabetes medication), methotrexate (arthritis/cancer treatment), antiretroviral drugs for HIV, phenytoin (seizure medication)
- Lifestyle: Chronic alcohol consumption, strict vegan diet without B12 supplementation, smoking
- Conditions: Recent blood transfusion, dehydration, high altitude living
- Supplements: Excessive folic acid supplementation without adequate B12
Factors That May Decrease Levels:
- Medications: Aspirin (chronic use), NSAIDs (can cause stomach bleeding), proton pump inhibitors (reduce iron absorption)
- Lifestyle: Vegetarian diet low in iron, excessive tea or coffee consumption with meals, frequent blood donation
- Conditions: Heavy menstrual periods, pregnancy, recent surgery, chronic infections
- Time of Day: MCH levels are generally stable throughout the day, unlike some other blood markers
How Is MCH Related to Other Tests?
MCH is like one piece of a puzzle that helps create the complete picture of your blood health. It's always measured alongside other red blood cell indices in your CBC.
Often tested alongside: MCV (red blood cell size), MCHC (hemoglobin concentration), RDW (variation in cell size), hemoglobin, hematocrit Part of: Complete Blood Count (CBC), Anemia Panel Ratio calculations: MCH helps calculate MCHC when combined with hematocrit values Follow-up tests: Iron studies, vitamin B12 levels, folate levels, ferritin, reticulocyte count
Frequently Asked Questions
How often should MCH be tested? For healthy adults, MCH is typically checked annually as part of a routine CBC. If you have a blood disorder or are being treated for anemia, your doctor may check it every 3-6 months or more frequently during treatment adjustments.
Can I improve my MCH levels naturally? Yes, if your abnormal MCH is due to nutritional deficiencies. Eating iron-rich foods (lean meats, beans, spinach), taking vitamin B12 supplements if deficient, and ensuring adequate folate intake can help normalize levels. Always work with your doctor before starting supplements.
Should I fast before an MCH test? No, fasting is not required for an MCH test or CBC. You can eat and drink normally before your blood draw, which makes this test very convenient.
How quickly can MCH levels change? MCH changes relatively slowly because red blood cells live about 120 days. After starting treatment for deficiencies, you might see improvements in 2-4 weeks, but full normalization often takes 2-3 months.
Next Steps After Your MCH Test
Questions to Ask Your Doctor:
- What do my MCH results mean for my overall health?
- Are my levels related to my symptoms?
- Do I need additional testing?
- Should we monitor this over time?
- Are there lifestyle changes that could help?
Download our MCH Doctor Questions Checklist
🔬 Ready to Track Your MCH Over Time?
Understanding a single MCH result is just the beginning. Our free Lab Analyzer tool helps you:
- Track how your MCH changes over time
- See how it relates to your other lab values
- Identify patterns your doctor might miss
- Get personalized insights based on your trends
[Upload Your Lab Report for Free Analysis →]