📋 At a Glance
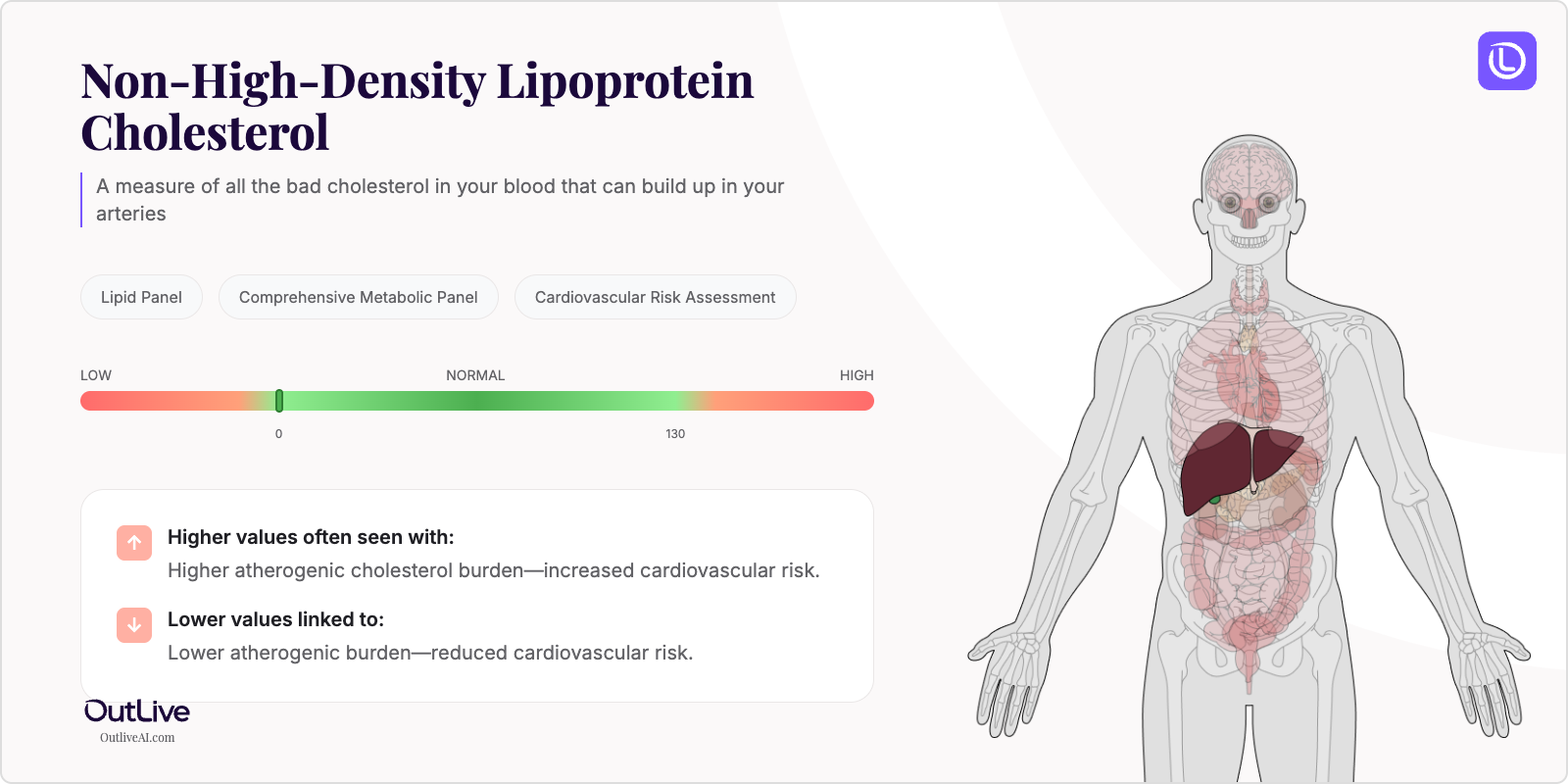
- What it is: A measure of all the "bad" cholesterol in your blood that can build up in your arteries
- Found in tests: Lipid Panel, Comprehensive Metabolic Panel, Cardiovascular Risk Assessment
- Normal range: Less than 130 mg/dL for most adults (varies by cardiovascular risk)
If you're looking at your lab results and wondering what non-HDL cholesterol means, you're in the right place. Think of non-HDL as the total of all the troublemaker cholesterol particles in your blood—like counting all the cars that could potentially cause a traffic jam on your arterial highways. Let's break down what your numbers mean in plain English.
Why Is Non-HDL Cholesterol Tested?
Your doctor orders a non-HDL cholesterol test as part of your routine lipid panel to get a complete picture of your heart health. This test has become increasingly important because it captures all the cholesterol types that can harm your arteries—not just the famous LDL cholesterol you've probably heard about. It's like getting a comprehensive security check rather than just looking at one potential threat.
Non-HDL cholesterol testing is especially valuable if you have diabetes, metabolic syndrome, or a family history of heart disease. Your doctor may also order it if you're experiencing symptoms like chest pain, shortness of breath, or if you've had unexplained fatigue. It helps monitor how well your cholesterol medications are working and whether lifestyle changes are making a difference.
This test matters because non-HDL cholesterol is actually a better predictor of heart disease risk than LDL cholesterol alone. It includes all the cholesterol-carrying particles that can stick to your artery walls, giving your healthcare team a more complete risk assessment.
What Does Non-HDL Cholesterol Do in Your Body?
Non-HDL cholesterol isn't actually a single substance—it's a calculation that represents all the cholesterol in your blood except for the "good" HDL cholesterol. Your body needs some cholesterol to build cells, make hormones, and produce vitamin D. But when non-HDL levels get too high, these particles can accumulate in your artery walls like sediment in a pipe, gradually narrowing the passageway for blood flow.
Your liver produces most of your cholesterol, but diet also plays a role. The non-HDL measurement includes LDL (low-density lipoprotein), VLDL (very low-density lipoprotein), and other cholesterol-rich particles. These particles travel through your bloodstream delivering fats to your cells, but excess amounts can deposit in your arteries, forming plaques that increase your risk of heart attack and stroke.
The beauty of measuring non-HDL cholesterol is its simplicity—it's calculated by subtracting your HDL cholesterol from your total cholesterol. This gives your doctor a single number that represents your overall "cholesterol burden" and helps guide treatment decisions more effectively than looking at individual cholesterol types alone.
What Do My Non-HDL Results Mean?
Normal Non-HDL Ranges
| Population | Normal Range | Optimal Range |
|---|---|---|
| Adult Male | < 130 mg/dL | < 100 mg/dL |
| Adult Female | < 130 mg/dL | < 100 mg/dL |
| Children (2-19 years) | < 120 mg/dL | < 110 mg/dL |
| High-risk adults* | < 100 mg/dL | < 70 mg/dL |
*High-risk includes those with diabetes, existing heart disease, or multiple cardiovascular risk factors
Note: Reference ranges may vary slightly between laboratories. Always compare your results to the range provided on your specific lab report.
What Does High Non-HDL Mean?
Common Causes:
- Diet high in saturated and trans fats (found in fried foods, processed snacks, fatty meats)
- Genetic conditions like familial hypercholesterolemia (inherited high cholesterol)
- Diabetes or poorly controlled blood sugar levels
- Hypothyroidism (underactive thyroid gland)
- Kidney disease or nephrotic syndrome
- Obesity and sedentary lifestyle
- Certain medications (steroids, some blood pressure drugs, HIV medications)
Possible Symptoms:
- Often no symptoms until complications develop
- Yellowish deposits around eyes or on skin (xanthomas)
- Gray-white rings around corneas (arcus senilis) in younger people
- Chest pain or pressure during physical activity
- Shortness of breath with exertion
When to Be Concerned: If your non-HDL cholesterol is above 160 mg/dL, you're at significantly increased risk for cardiovascular disease. Levels above 190 mg/dL require immediate medical attention and likely medication. Any chest pain, sudden shortness of breath, or signs of stroke (facial drooping, arm weakness, speech difficulties) warrant emergency care regardless of your cholesterol levels.
What Does Low Non-HDL Mean?
Common Causes:
- Hyperthyroidism (overactive thyroid)
- Malnutrition or malabsorption disorders
- Chronic liver disease or cirrhosis
- Certain cancers or blood disorders
- Genetic conditions affecting cholesterol production
- Excessive use of cholesterol-lowering medications
- Severe infections or inflammatory conditions
Possible Symptoms:
- Usually no symptoms from low cholesterol itself
- Fatigue or weakness (if related to underlying condition)
- Unexplained weight loss
- Poor wound healing
- Depression or mood changes (in very low levels)
When to Be Concerned: While low non-HDL cholesterol is generally not as concerning as high levels, values below 40 mg/dL may indicate an underlying health issue that needs investigation. If accompanied by unexplained weight loss, persistent fatigue, or other concerning symptoms, discuss with your doctor promptly.
What Can Affect My Non-HDL Levels?
Factors That May Increase Levels:
- Medications: Corticosteroids, thiazide diuretics, beta-blockers, oral contraceptives, protease inhibitors
- Lifestyle: High saturated fat diet, excessive alcohol consumption, smoking, lack of exercise
- Conditions: Pregnancy (temporary increase), winter months (seasonal variation), recent weight gain
- Supplements: Anabolic steroids, high-dose vitamin A
Factors That May Decrease Levels:
- Medications: Statins, fibrates, niacin, PCSK9 inhibitors, bile acid sequestrants
- Lifestyle: Plant-based diet, regular aerobic exercise, weight loss, moderate alcohol consumption
- Conditions: Acute illness or infection, hyperthyroidism, recent surgery
- Time of Day: Levels can vary by 10% throughout the day
How Is Non-HDL Cholesterol Related to Other Tests?
Non-HDL cholesterol is calculated from your total cholesterol and HDL cholesterol values, making it an integral part of your lipid panel. It correlates closely with apolipoprotein B (apoB) levels, another marker of cardiovascular risk, but is simpler and less expensive to obtain.
Often tested alongside: Total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides Part of: Lipid Panel, Cardiovascular Risk Assessment Ratio calculations: Non-HDL/HDL ratio provides additional risk stratification Follow-up tests: If abnormal, your doctor may order thyroid function tests, liver enzymes, fasting glucose, or apolipoprotein B
Frequently Asked Questions
How often should non-HDL be tested? For healthy adults, every 4-6 years is typically sufficient. If you have risk factors or are on cholesterol medication, your doctor may recommend testing every 3-12 months until levels are controlled, then annually.
Can I improve my non-HDL levels naturally? Yes! Losing 5-10% of body weight, exercising 150 minutes weekly, replacing saturated fats with unsaturated fats, adding soluble fiber (oats, beans, apples), and limiting refined sugars can significantly lower non-HDL cholesterol.
Should I fast before a non-HDL test? One advantage of non-HDL cholesterol is that fasting isn't required for accurate results, unlike LDL cholesterol. You can eat normally before the test.
How quickly can non-HDL levels change? Diet and exercise changes can show improvements in 6-8 weeks. Cholesterol medications typically show effects within 4-6 weeks. Significant weight loss may take 3-6 months to fully impact your levels.
Next Steps After Your Non-HDL Test
Questions to Ask Your Doctor:
- What do my non-HDL results mean for my overall cardiovascular risk?
- Are my levels related to my family history or current symptoms?
- Do I need additional testing like apoB or a coronary calcium scan?
- Should we monitor this more frequently given my risk factors?
- What specific dietary changes would be most helpful for my situation?
Download our Non-HDL Cholesterol Doctor Questions Checklist
🔬 Ready to Track Your Non-HDL Cholesterol Over Time?
Understanding a single non-HDL result is just the beginning. Our free Lab Analyzer tool helps you:
- Track how your non-HDL changes over time
- See how it relates to your other lab values
- Identify patterns your doctor might miss
- Get personalized insights based on your trends
[Upload Your Lab Report for Free Analysis →]