📋 At a Glance
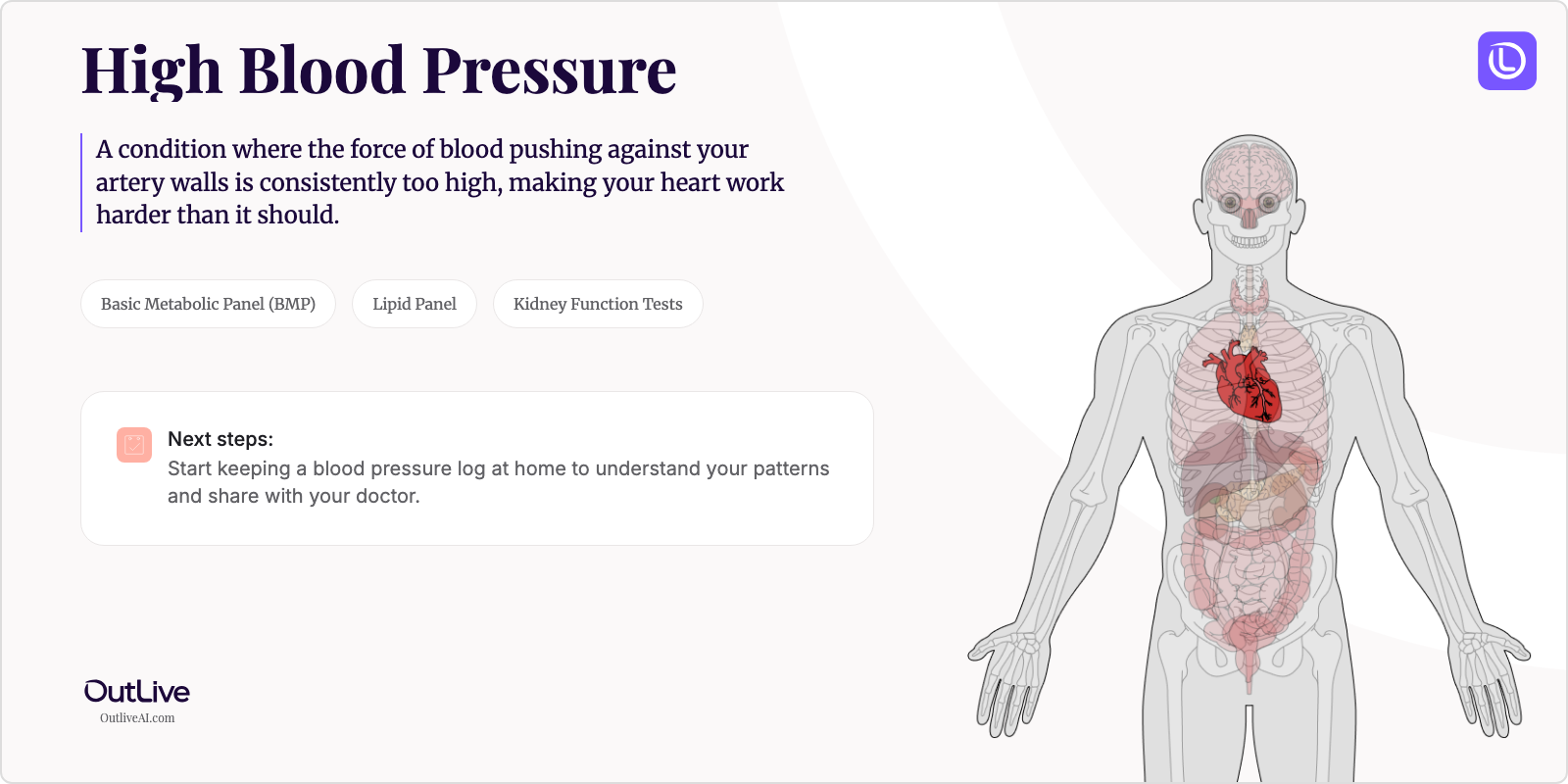
- What it is: A condition where the force of blood pushing against your artery walls is consistently too high, making your heart work harder than it should.
- Key lab tests: Basic Metabolic Panel (BMP), Lipid Panel, and Kidney Function Tests
- Your first goal: Start keeping a blood pressure log at home to understand your patterns and share with your doctor.
Receiving a new diagnosis for High Blood Pressure can be overwhelming. You might be feeling anxious, confused, and unsure of what comes next. That's completely normal. This guide is here to help you understand your condition in simple terms, know which lab tests matter most, and feel prepared for your next steps.
First, Take a Breath: What is High Blood Pressure in Simple Terms?
Think of your blood vessels as garden hoses and your heart as the water pump. High blood pressure means the pump is pushing water through the hoses with too much force. Over time, this extra pressure can damage the hoses (your blood vessels) and strain the pump (your heart). The good news? Unlike a broken garden hose, your body can heal and adapt when we reduce that pressure. High blood pressure is often called the "silent killer" because you usually can't feel it happening, but catching it early—like you have—means you can take control before any serious damage occurs.
Understanding Your Diagnosis: The Key Lab Tests
This is the most important section. These are the tests your doctor will use to understand your high blood pressure and monitor how well your treatment is working.
Key Tests for High Blood Pressure:
- Creatinine: This test checks how well your kidneys are filtering waste from your blood, since high blood pressure can damage these vital organs over time.
- Cholesterol Panel: Measures different types of fats in your blood that can team up with high blood pressure to increase your risk of heart disease.
- Glucose: Checks your blood sugar levels because diabetes and high blood pressure often go hand-in-hand and multiply each other's risks.
- Potassium: Monitors an essential mineral that helps regulate blood pressure and can be affected by blood pressure medications.
Your First Specialist Appointment: What to Ask
What to Expect: You'll likely continue seeing your primary care doctor for high blood pressure management, though they may refer you to a cardiologist if your case is complex. During your appointment, they'll review your blood pressure readings, discuss your medical history and lifestyle, perform a physical exam, and create a personalized treatment plan. Don't be surprised if they want to check your blood pressure multiple times—this gives them a better picture of your true levels.
Questions to Ask Your Doctor:
- "What are my actual blood pressure numbers, and what should my target numbers be?"
- "Do I need medication right away, or can we try lifestyle changes first?"
- "How often should I check my blood pressure at home, and what type of monitor do you recommend?"
- "Are there specific foods I should avoid or add to my diet?"
- "What side effects should I watch for if you're prescribing medication?"
Download our [Checklist of Questions to Ask Your High Blood Pressure Specialist](# to feel prepared.
How to Track Your Journey
Tracking your High Blood Pressure journey is crucial for understanding how your treatment is working and spotting important trends. Here's what you should monitor:
Symptoms to Track:
- Headaches (especially in the morning)
- Dizziness or feeling lightheaded
- Chest pain or shortness of breath
- Vision changes or blurry vision
- Nosebleeds (if frequent)
Lab Results to Monitor:
- Kidney function tests (creatinine, eGFR) - Every 6-12 months
- Cholesterol levels - Annually or as directed
- Blood glucose - Annually if normal, more often if elevated
- Electrolytes (sodium, potassium) - Every 6 months if on medication
Why Tracking Matters: Your blood pressure can vary throughout the day and in response to stress, diet, and activity. By tracking patterns over time, you and your doctor can see if treatments are working, identify triggers that spike your pressure, and catch any medication side effects early. This information helps fine-tune your treatment plan for the best results.
Next Steps After Your Diagnosis
Immediate Actions (This Week):
- Purchase a home blood pressure monitor and learn how to use it correctly
- Start a simple log of your daily blood pressure readings (morning and evening)
- Schedule any follow-up lab tests your doctor recommended
Short-term Goals (Next Month):
- Establish a routine for checking and recording your blood pressure
- Begin implementing dietary changes like reducing sodium intake
- Start a gentle exercise routine (even 15-minute daily walks help)
Long-term Management:
- Build sustainable lifestyle habits that support healthy blood pressure
- Maintain regular check-ups and lab work to monitor your progress
- Learn to recognize how stress affects your blood pressure and develop coping strategies
Frequently Asked Questions
How quickly can I expect to feel better? Many people with high blood pressure don't feel "sick" to begin with, which can make progress hard to notice. If you had symptoms like headaches, you might see improvement within 2-4 weeks of treatment. The real benefits—protecting your heart, brain, and kidneys—happen gradually over months and years.
Will I need to change my diet? Most likely, yes, but the changes don't have to be drastic. Focus on reducing sodium (aim for less than 2,300mg daily), eating more fruits and vegetables, and limiting processed foods. The DASH diet is specifically designed for people with high blood pressure and can lower your numbers within just two weeks.
How often will I need to see my doctor? Initially, you'll likely have appointments every 1-3 months until your blood pressure is controlled. Once stable, most people see their doctor every 3-6 months. You'll need annual lab work at minimum, though some tests may be needed more frequently.
Can I still exercise/work/travel? Absolutely! In fact, regular exercise is one of the best treatments for high blood pressure. Start slowly and build up gradually. Most people can continue working and traveling normally, though you should always pack extra medication when traveling and know how to check your blood pressure while away from home.
When to Seek Immediate Medical Attention
Contact your doctor immediately if you experience:
- Severe headache with confusion or difficulty speaking
- Chest pain or pressure that doesn't go away
- Blood pressure reading over 180/120 (this is a hypertensive crisis)
- Sudden vision loss or severe blurry vision
- Difficulty breathing or severe shortness of breath
- Severe anxiety with rapid heartbeat
🔬 Ready to Organize Your Health Journey?
Understanding your condition is the first step. Our free Lab Analyzer tool helps you:
- Track all your lab results for High Blood Pressure in one place
- Spot important trends over time
- Generate personalized questions for your doctor
[Upload Your Lab Report for Free Analysis →]