📋 At a Glance
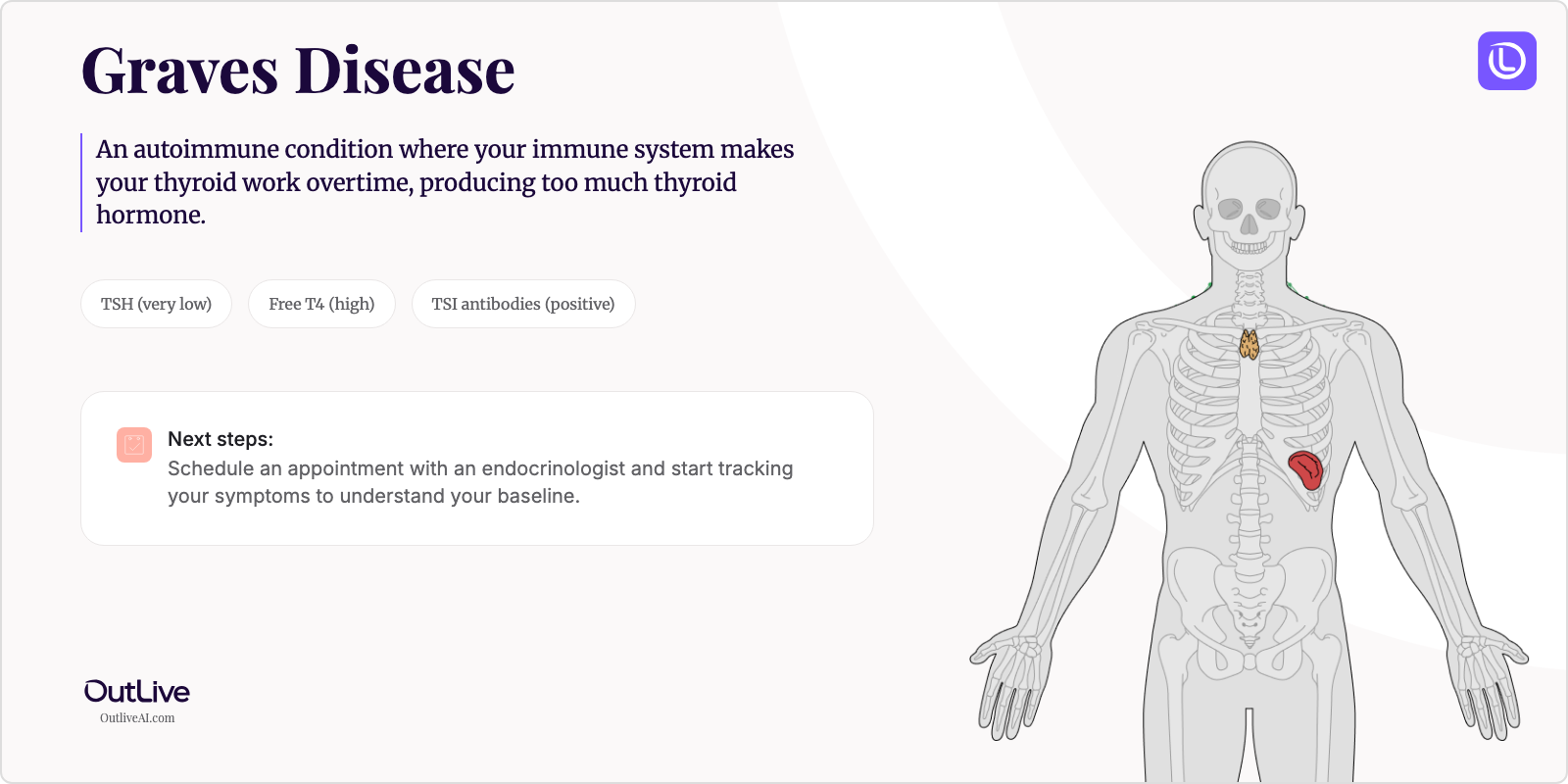
- What it is: An autoimmune condition where your immune system makes your thyroid work overtime, producing too much thyroid hormone.
- Key lab tests: TSH (very low), Free T4 (high), TSI antibodies (positive)
- Your first goal: Schedule an appointment with an endocrinologist and start tracking your symptoms to understand your baseline.
Receiving a new diagnosis for Graves' Disease can be overwhelming. You might be feeling anxious, confused, and unsure of what comes next. That's completely normal. This guide is here to help you understand your condition in simple terms, know which lab tests matter most, and feel prepared for your next steps.
First, Take a Breath: What is Graves' Disease in Simple Terms?
Imagine your thyroid gland as your body's thermostat—it controls how fast or slow everything runs, from your heartbeat to your metabolism. In Graves' Disease, your immune system gets confused and creates special antibodies that essentially "jam" this thermostat in the "high" position. Your thyroid then produces way too much hormone, making everything in your body run faster than it should—like a car engine that's constantly revving. The good news? This is one of the most treatable thyroid conditions, and with proper management, most people with Graves' Disease lead completely normal lives.
Understanding Your Diagnosis: The Key Lab Tests
This is the most important section. These are the lab tests your doctor uses to diagnose and monitor your Graves' Disease. Understanding them helps you become an active partner in your care.
Key Tests for Graves' Disease:
- TSH (Thyroid Stimulating Hormone): This is your body's "thyroid control signal"—in Graves' Disease, it's typically very low or undetectable because your thyroid is already working overtime without needing any signals.
- Free T4 (Thyroxine): This measures the actual thyroid hormone circulating in your blood—it's usually elevated in Graves' Disease, causing your symptoms like rapid heartbeat and weight loss.
- TSI (Thyroid Stimulating Immunoglobulin): These are the specific antibodies your immune system makes in Graves' Disease—a positive result confirms your diagnosis and helps distinguish Graves' from other thyroid conditions.
- Free T3 (Triiodothyronine): This is the active form of thyroid hormone—it's often elevated and helps your doctor understand the severity of your hyperthyroidism.
Your First Specialist Appointment: What to Ask
What to Expect: You'll be seeing an endocrinologist—a hormone specialist who treats thyroid conditions every day. They'll review your lab results, perform a physical exam (checking your thyroid, eyes, and reflexes), and discuss treatment options. The appointment typically lasts 30-45 minutes, and you'll leave with a clear treatment plan. Don't worry if you feel overwhelmed—it's normal, and your doctor expects lots of questions.
Questions to Ask Your Doctor:
- "What are my three treatment options (medication, radioactive iodine, surgery) and which do you recommend for me specifically?"
- "How often will I need blood work, and what numbers are we aiming for?"
- "What symptoms should improve first, and how long before I start feeling better?"
- "Are there any lifestyle changes or dietary modifications that could help my symptoms?"
- "Should I see an eye specialist, even if I don't have eye symptoms yet?"
Download our [Checklist of Questions to Ask Your Graves' Disease Specialist](# to feel prepared.
How to Track Your Journey
Tracking your Graves' Disease journey is crucial for understanding how your treatment is working and spotting important trends. Here's what you should monitor:
Symptoms to Track:
- Heart rate (especially resting heart rate in the morning)
- Weight changes (weekly weigh-ins at the same time of day)
- Energy levels and sleep quality (rate them 1-10 daily)
- Anxiety or mood changes
- Any eye irritation, bulging, or vision changes
Lab Results to Monitor:
- TSH and Free T4 - Every 4-6 weeks initially, then every 2-3 months once stable
- Free T3 - Every 4-6 weeks initially if elevated
- Liver function tests - Every 2-3 months if on methimazole
- Complete blood count - Periodically if on antithyroid medications
Why Tracking Matters: Your thyroid levels can fluctuate during treatment, and symptoms don't always match lab results perfectly. By tracking both, you and your doctor can fine-tune your treatment faster, catch side effects early, and celebrate improvements. Many patients find that seeing their progress on paper helps reduce anxiety and gives them a sense of control.
Next Steps After Your Diagnosis
Immediate Actions (This Week):
- Schedule an appointment with an endocrinologist if you haven't already
- Start a symptom diary—even simple notes on your phone work
- Inform close family members about your diagnosis and what support you might need
- Fill your prescription if medication was started
Short-term Goals (Next Month):
- Establish care with an ophthalmologist for baseline eye exam
- Learn to check your resting heart rate and do it daily
- Join a Graves' Disease support group (online or local)
- Create a system for organizing your lab results
Long-term Management:
- Regular monitoring every 2-3 months once stable
- Annual eye exams even after remission
- Understanding your personal triggers for flare-ups
- Building a sustainable lifestyle that supports thyroid health
Frequently Asked Questions
How quickly can I expect to feel better? Most people start noticing improvements within 2-4 weeks of starting antithyroid medication. Heart rate often improves first, followed by anxiety and tremors. Full symptom resolution typically takes 2-3 months, though everyone's timeline is different.
Will I need to change my diet? While there's no specific "Graves' Disease diet," eating regular meals with adequate calories is important since your metabolism is running high. Some patients find limiting caffeine helps with heart palpitations and anxiety. If you're on antithyroid medication, you don't need to avoid iodine-rich foods.
How often will I need to see my doctor? Initially, expect appointments every 4-6 weeks until your levels stabilize. Once stable on treatment, visits typically space out to every 2-3 months, then eventually every 6 months. You'll need more frequent monitoring if changing treatments.
Can I still exercise/work/travel? Yes to all three, with some modifications. Start with gentle exercise and gradually increase as your heart rate normalizes. Most people can work, though you might need accommodations initially. Travel is fine—just pack extra medication and know where to get medical care at your destination.
When to Seek Immediate Medical Attention
Contact your doctor immediately if you experience:
- Fever with sore throat (could indicate a rare but serious medication side effect)
- Severe eye pain, vision changes, or sudden eye bulging
- Chest pain, irregular heartbeat, or heart rate over 140 at rest
- Confusion, high fever, and extreme agitation (signs of thyroid storm—call 911)
- Severe abdominal pain or yellowing of skin/eyes
🔬 Ready to Organize Your Health Journey?
Understanding your condition is the first step. Our free Lab Analyzer tool helps you:
- Track all your lab results for Graves' Disease in one place
- Spot important trends over time
- Generate personalized questions for your doctor
[Upload Your Lab Report for Free Analysis →]